Primary or secondary infertility
No pregnancy even after 1 year of regular unprotected sex (when female age is /= 35 years).
Primary Infertility is when a couple has not conceived before.
Secondary Infertility is when a couple has a child/conceived before and now they have difficulty in conceiving.
Infertility evaluation must begin with both, female and male partner's detailed history of infertility and previous treatments taken. This should be followed by checkup, some tests and sonography to find any pathology. As a doctor we need assurance of having a good sexual life for that couple, proper egg formation and release (female partner) + healthy sperms in semen (male partner) and when needed we need to check the patency of fallopian tubes (female partner).
Natural conception
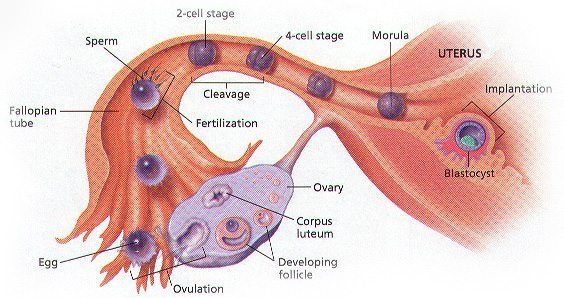
Naturally conception happens when a female releases an egg from her ovary (Ovulation), which enters into that side of the fallopian tube where it meets a sperm. Sperms are present in the ejaculated semen during intercourse (sex). When that sperm fertilizes an egg in the fallopian tube, an embryo is formed. That embryo travels on its way to the uterus from the tube to get itself implanted on the endometrial lining (innermost lining of the uterus). This way pregnancy happens.
So, for successful pregnancy to happen there are many steps which can go wrong and hence we as a doctor should check all the following parameters in the evaluation of a couple who can not get pregnancy even after 12 months of regular unprotected timed sex.
Female partner evaluation
- To check Ovarian Reserve (egg number/ quantity in the ovaries)
- Confirmation of ovulation (egg release) in the ovaries
- Formation of proper endometrial lining in the uterus
- Confirm tubal (fallopian tube) patency
Male partner evaluation
Confirm normal semen parameter
Female partner evaluation
(1) To check Ovarian Reserve (egg number/ quantity in the ovaries)
- Ovarian Reserve means total egg production capacity of ovaries/ total number of eggs/ egg quantity.
- A female has a fixed number of eggs in her ovaries even before her birth, when she is in her mother’s womb. Those eggs get depleted every month whether she menstruates or not, like even during her prepubertal life.
- It means it is a biological clock which is ticking all the time. After a certain age (generally around 45-50 years of age)she exhausts her egg reserve and that is called menopause, which is an end of her fertility; end of her ability to get pregnant with her own eggs.
- Age has an impact not only on egg number but also on its quality.
- That is why documenting ovarian reserve is of utmost importance not only for infertile women but also for a woman who comes for preconception counselling. Because this determines the timeline and urgency of her infertility treatment, like how fast she should be pregnant or at least she can be given the option of her egg freezing.
- Ovarian reserve can be checked by transvaginal sonography on initial days of menses (2nd/3rd day) by checking her Antral Follicle Count (AFC) or by a blood test called Anti Mullerian Hormone (AMH) at any day of menses.
(2) Confirmation of ovulation (egg release) in the ovaries
- Woman with a regular menstruation cycle of 28 days is ovulating ~14th day of her cycle. It means regular menstruation is an indirect indication of her regular and timed ovulation.
- After ovulation - egg has 24 hour lifespan during which it has to be penetrated by ejaculated sperm in the fallopian tube and fertilize it or else it will degenerate on its own.
- So, Ovulation time is the time during which a couple should have sexual intercourse to fertilize the egg and eventually have a successful pregnancy.
- Irregular menstruation/periods indicates some ovulation issue in that woman.
- If a woman gets her periods every 45-60 days interval instead of 28-30 days, that suggests delayed egg formation and hence delayed ovulation. Hence, prediction of ovulation is very difficult for that couple. For this issue a couple should consult their Gynecologist/ Infertility Specialist doctor for serial sonography, necessary tests and treatment to facilitate ovulation and in turn pregnancy.
- Some women also suffer from anovulation (no ovulation), which is commonly associated with PCOD (polycyctic ovarian disorder). These women have either no periods without medicines or very long intervals between periods (approx 3-4 months). These women will be benefited after consultation, examination and treatment in the form of oral or injectable medicines (Ovulation Induction). Some may require laparoscopic ovarian drilling or IVF (In-vitro Fertilization).
(3) Formation of proper endometrial lining in the uterus
- Endometrial lining is the innermost layer of the uterus where embryo implants to have a successful pregnancy. So, properly formed and receptive endometrium is a very important factor to be considered
- Endometrial thickness, pattern and its vascularity; all are associated with pregnancy.
- Endometrial thickness is a simple non-invasive test to determine its receptivity and hence it is widely used among all gynecologists and infertility specialists to know receptivity. More than 7 mm triple line endometrial thickness on sonography at the time of fully dominant follicle(s) is to be considered as good receptive endometrium.
- Thin endometrium (<7 mm) should be evaluated thoroughly and to be treated to achieve good pregnancy rates
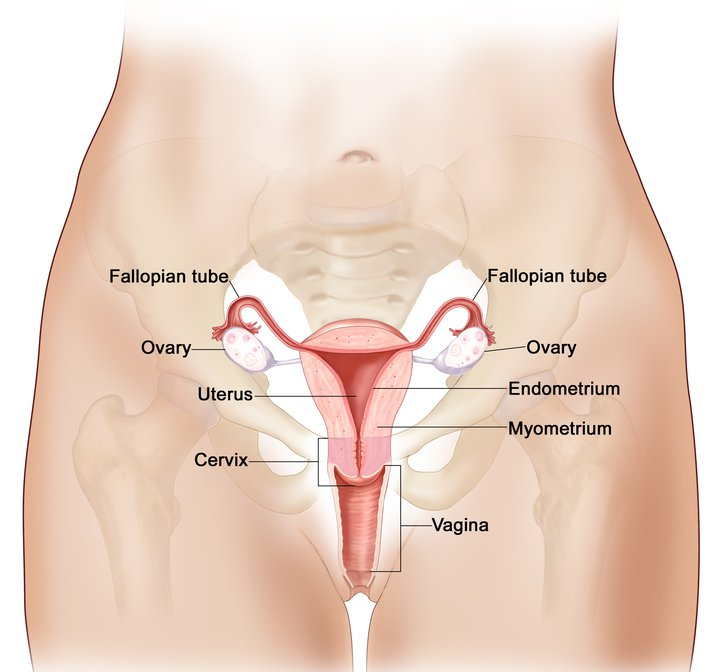
(4) Confirm tubal (fallopian tube) patency
- Fallopian tubes are not visualised in sonography unless it is dilated/diseased
- So, we need some tests to check their patency like Rubin’s test (RT), Hysterosalpingography (HSG), Sonosalpingography (SSG) or Laparoscopy.
- RT, HSG and SSG are indirect and non-invasive tests but have many limitations in terms of side effects and its sensitivity and specificity.
- Laparoscopy is considered to be the gold standard in diagnosing any anatomical abnormalities of female reproductive organs as it means direct visualization of those structures plus simultaneous surgical correction is also possible when needed.
Male partner evaluation
Confirm normal semen parameter
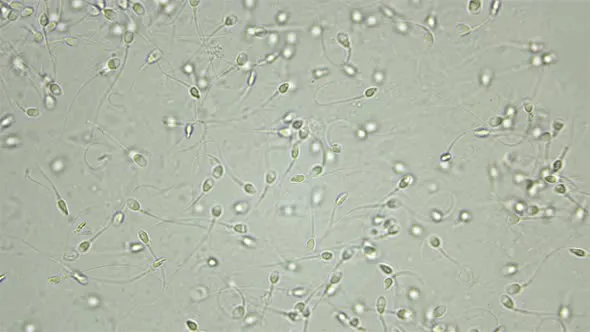
- Proper semen deposition in vagina and normal semen parameters are the two important factors to be fulfilled by male partner.
- Sperm count, motility and morphology (~appearance) are the three most important semen parameters to be studied in semen analysis in the laboratory.
- According to WHO 2010, sperm count >15 million per ml, progressive motility of >32% and >4% normal sperm morphology is considered as normal semen to achieve pregnancy.
- Any parameters less than this range should be investigated thoroughly and treated on time.